Public Health
When Should You Go to the ER vs Urgent Care vs Primary Care?
Understanding where to turn for the right medical care is important. Maryland hospitals and health systems are open 24/7/365 and care for everyone who comes through their doors—regardless of ability to pay.
However, often there are more appropriate care settings. Knowing where to go decreases the amount of time a patient waits for care for themselves, their family, their friends, and everyone in their community.
Know Where To Go: The Right Care, in the Right Setting

Primary Care
Provider
Establishing a long-term relationship with a primary care provider gives you a chance to be healthier, get more personalized and comprehensive care. Go to a primary care provider for:
Preventive Care: Regular check-ups, vaccinations, and screenings
Chronic Conditions: Management of ongoing health issues

Telehealth
Consultations
Virtual care is accessible right from the comfort of your home, saves time, and reduces risk of exposure to other people. It’s perfect for non-urgent matters such as:
Common Ailments: Colds, allergies, mild infections, lingering symptoms, diarrhea, and others
Medication Refills: When a physical visit isn’t necessary

Urgent Care
Services
When you don’t have life threatening injuries or illness, urgent care is quicker, convenient, and efficient for issues like these:
Minor Injuries: Sprains, breaks, minor fractures, cuts requiring stitches
Illnesses: Fever, flu symptoms, and infections that need prompt attention

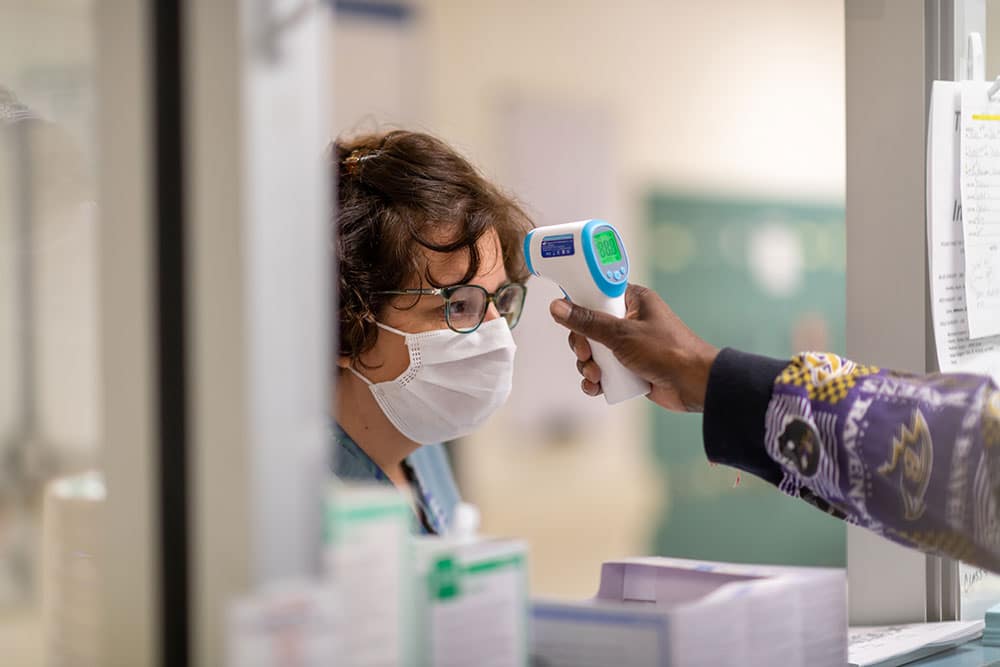
Emergency Room
Services
Emergency departments are equipped to handle critical situations and provide 24/7 care. The American College of Emergency Physicians and Johns Hopkins Medicine recommend seeking immediate emergency care for these concerns:
Remember: Emergency departments triage all patients as they come in, and those with the most serious medical needs take priority.
Life-threatening or conditions requiring immediate attention inclue:
- Difficulty breathing, shortness of breath
- Chest or upper belly pain or pressure lasting 2 minutes or more
- Fainting, sudden dizziness, weakness
- Changes in vision
- Confusion or changes in mental status
- Any sudden or severe pain
- Uncontrolled bleeding
- Severe or persistent vomiting or diarrhea
- Coughing or vomiting blood
- Suicidal or homicidal feelings
- Difficulty speaking, or numbness or weakness in any part of your body
- Unusual belly pain
- Poisoning
- Drug overdose
- Loss of consciousness
- Major burn
- Spinal cord, head, or brain injury
- Severe allergic reaction
- A fast heartbeat (more than 120 to 150 beats per minute) at rest, especially if associated with shortness of breath or feeling faint
- A broken bone with skin protruding through the skin
- Drowning
Emergency Guide: Know Where to Go
This guide helps Marylanders Know Where to Go to get the care they need, when they need it.

Call or see your primary care provider (PCP) for your regular medical needs or non-urgent conditions. Go for common or mild issues urgently needing to be treated, if your primary care provider is not available.
Go for common or mild issues urgently needing to be treated, if your primary care provider is not available.

Call/video to address non-urgent health concerns. Go only for severe life and limb-threatening conditions needing more care than your PCP or urgent care can offer.
Go only for severe life and limb-threatening conditions needing more care than your PCP or urgent care can offer.

Resources for Members
When visiting the Emergency Room, all patients are treated based on their degree of illness, not on a first-come, first-serve basis. If your condition isn’t life-threatening, visit an urgent care center or contact your primary care provider.
Learn more https://t.co/Ei7FoAReml pic.twitter.com/dtvukroZDr
— UM UCH (@UpperChesapeake) October 30, 2024